Mitochondrial DNA Mutations and Cancer
A recent paper in Science Advances describes the findings of a research team led by Mondira Kundu, MD, PhD, at St. Jude Children’s Research Hospital. The study investigates how mitochondrial (mt) DNA mutations influence leukemia pathology. Unexpectedly, their research showed that a moderate burden of mtDNA mutations can enhance the development of leukemia. They also show that cancer can be re-initiated by inhibiting a specific enzyme in cells carrying a high burden of mtDNA mutations.
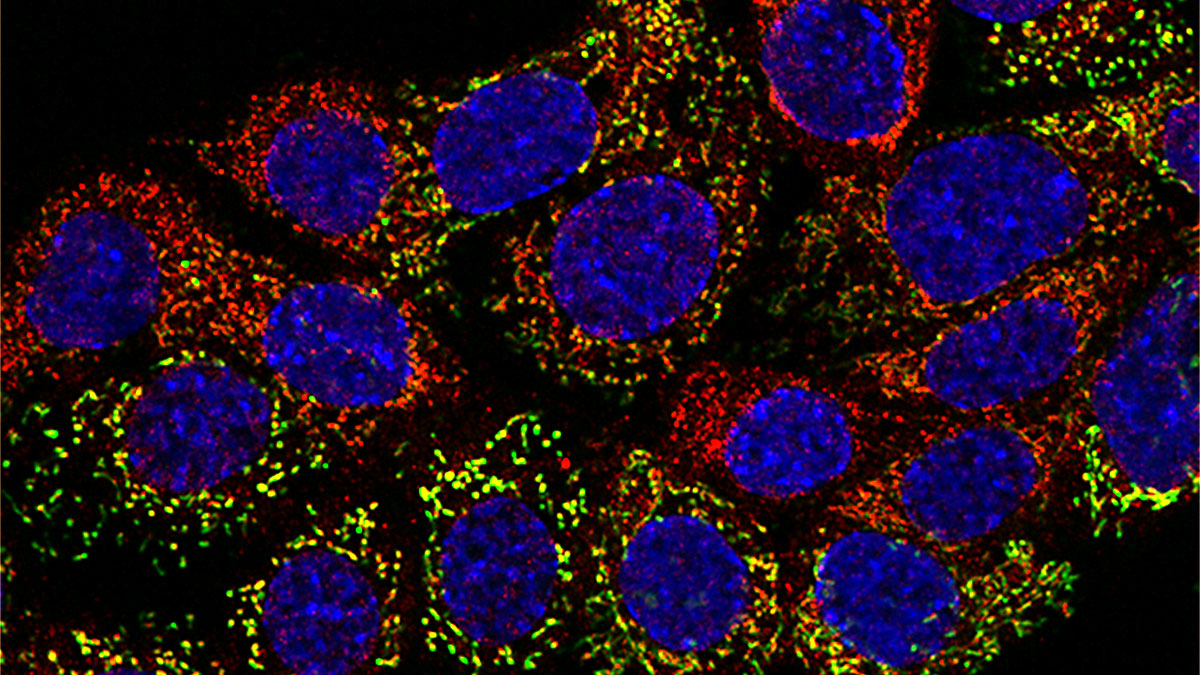
Cancers are highly energy dependent, with the mitochondria serving as the cell’s main energy producers. While most research into this connection has focused on mutations in nuclear DNA that affect mitochondrial function, Dr. Kundu’s team explored whether mutations directly in the mtDNA contribute to tumor development.
The researchers began with three lines of mice expressing a mutant exonuclease-inactive mitochondrial DNA polymerase (Polgmut) that lacks accurate proofreading ability. These lines possess either zero (Polgwt/wt), one (Polgwt/mut), or two (Polgmut/mut) copies of the mutated allele, resulting in a graded accumulation of mtDNA mutations. Hematopoietic progenitor cells (HPCs) were isolated from these mice and engineered to express NMyc, a member of the MYC family of transcription factors. Members of the MYC family are commonly dysregulated in many blood cancers, such as leukemia. By transplanting these HPCs into irradiated recipient mice, the team assessed the impact of different levels of mtDNA mutations on cellular metabolism and cancer development.
The findings were unexpected: while metabolism was reduced in mice with either heterozygous or homozygous mutant cells, mice with a moderate mutation load (Polgmut/wt) were more prone to tumor formation than those with a high mutation load (Polgmut/mut). Metabolic plasticity was affected by the number of mtDNA mutations and was critical to the tumorigenic potential of the HPCs. In essence, a moderate number of mutations makes cells more metabolically flexible and more carcinogenic, whereas extensive mutations diminish both their metabolic flexibility and cancerous potential.
Conversation with Dr. Kundu
MitoWorld. Your results are unexpected. Do you have any thoughts on why the partially damaged mitochondria would be beneficial to the cancer? Yes, it appears that partially damaged mitochondria create a unique metabolic environment that cancer cells can exploit. Moderate mitochondrial dysfunction may allow for metabolic reprogramming—enhancing glycolysis and other pathways that support rapid cell growth—without fully compromising energy production. This balance may give cancer cells a survival and growth advantage.
MitoWorld. Can you speculate on how the damaged mitochondria are able to increase their metabolic support for the tumors? Damaged mitochondria may trigger adaptive responses in cancer cells, activating alternative metabolic pathways and stress responses. For instance, partial mitochondrial dysfunction can increase the reliance on glycolysis (the Warburg effect) and other biosynthetic pathways, thereby supporting both energy needs and the synthesis of cellular building blocks required for proliferation. The cells remain metabolically flexible, which is crucial for tumor growth.
MitoWorld. You note both similar and different results with this mutation and different cancers. To what would you attribute those varying results? The impact of mtDNA mutations likely depends on the tissue context and the specific metabolic requirements of different cancers. Some tumors may be more resilient to mitochondrial dysfunction, while others are more dependent on intact mitochondrial metabolism. Additionally, the interplay between mtDNA mutations and nuclear gene mutations can vary, influencing how cells adapt metabolically and whether they become more or less tumorigenic.
MitoWorld. Your results show that inhibiting pyruvate dehydrogenase kinase improved the ability of the homozygous mutant to cause tumors. Does this observation have any therapeutic implications? While our findings are not immediately translatable to therapy, they do highlight the critical role of metabolic plasticity in leukemogenesis. The fact that inhibiting pyruvate dehydrogenase kinase (PDK) restored the proliferative capacity of homozygous mutant HPCs suggests that metabolic pathways can profoundly influence tumor development. This raises the possibility that targeting metabolic enzymes like PDK could one day be leveraged to modulate cancer cell growth, either by restricting the metabolic flexibility of cancer cells or by exploiting specific metabolic vulnerabilities. However, more research is needed, especially since the mutation burden in human leukemias typically comes from single mtDNA mutations, unlike the mouse model, where the burden comes from the cumulative effect of many mutations.
MitoWorld. What do you see as the next steps to follow up on this work? The next step is to introduce specific mtDNA mutations into primary cells and then add oncogenes. This will allow us to examine how individual mtDNA mutations—and their allele fractions—impact tumorigenesis. By better modeling the mutation patterns seen in human cancers, we can determine whether particular mtDNA mutations or metabolic states make cancer cells more susceptible to targeted metabolic therapies. Ultimately, this line of research could guide the development of new therapeutic strategies that exploit the metabolic dependencies created by mtDNA mutations in cancer cells.
MitoWorld. What attracted you to the study of mitochondria? As a hematopathologist, I have a strong interest in hematologic diseases, but my research has always spanned a variety of biological systems. My interest in mitochondria began during my postdoctoral fellowship in Craig Thompson’s lab, where I used red blood cell maturation as a model to study mitophagy—the process by which cells selectively remove damaged or superfluous mitochondria. That experience highlighted for me how central mitochondrial function and dysfunction are to cell biology and disease, including cancer. I am particularly intrigued by how cells sense and respond to mitochondrial dysfunction—especially when it’s caused by mtDNA mutations—and how these adaptive pathways can contribute to cancer development. Understanding the complex interplay between mitochondrial function and cellular responses not only deepens our knowledge of cancer biology but also points to new possibilities for therapeutic intervention.
Reference
Li-Harms X, Lu J, Fukuda Y, Lynch J, Sheth A, Pareek G, Kaminski MM, Ross HS, Wright CW, Smith AL, Wu H, Wang Y-D, Valentine M, Neale G, Vogel P, Pounds S, Schuetz JD, Ni M, Kundu M (2025) Somatic mtDNA mutation burden shapes metabolic plasticity in leukemogenesis. Science Advances 11(1): eads8489.