Mitochondria in Space
In a preprint article currently under review1, “Guardians of the mitochondria: Space mitochondria 2.0 systemic analysis reveals bioenergetic dysregulation across species,” a research team led by Afshin Beheshti (Director of Center for Space Biomedicine, Associate Director of the McGowan Institute for Regenerative Medicine, and Professor of Surgery and Computational and Systems Biology at the University of Pittsburgh) with co-senior author Chris Mason (WorldQuant Professor at Weill Cornell Medicine) explores the broad impacts of spaceflight on mitochondrial biology in humans and across a range of animal species to identify consistent effects of space exposure on the organelle and its influence on human health.
Astronauts returning to Earth after extended time in space suffer a number of stressors, including bone and muscle loss, cardiovascular and renal issues, circadian rhythm disruptions, potential long-term cancer risks, and ocular disorders. These health effects are thought to be caused by some combination of exposure to higher levels of radiation and reduced gravity. However, the exact mechanisms of how the conditions of space travel manifest in the physical symptoms in astronauts and other organisms are still unclear.
Previous work by Mason and Beheshti, including the “NASA Twins Study” and the “Space Omics and Medical Atlas,” measured biological characteristics in twin astronauts, Mark and Scott Kelly2 and then compared them to many additional cohorts and missions. The landmark Twins study tracked the astronauts over 340 days, while one flew on the international space station and the other remained on Earth. Surprisingly, the investigators identified mitochondrial respiration as one of the first and most important biological processes to be disrupted by spaceflight.
This new report aims to expand upon and generalize the prior findings by extracting mitochondrial function data from several studies of space exposure in a range of species, including humans (Guarnieri et al., in review). This large-scale, multi-institute study integrates an impressive collection of multi-omics data from humans, rodents, and other organisms before, during, and after returning from space. This rich dataset enables the authors to draw broader conclusions about how the mitochondria of people or animals will respond to spaceflight.
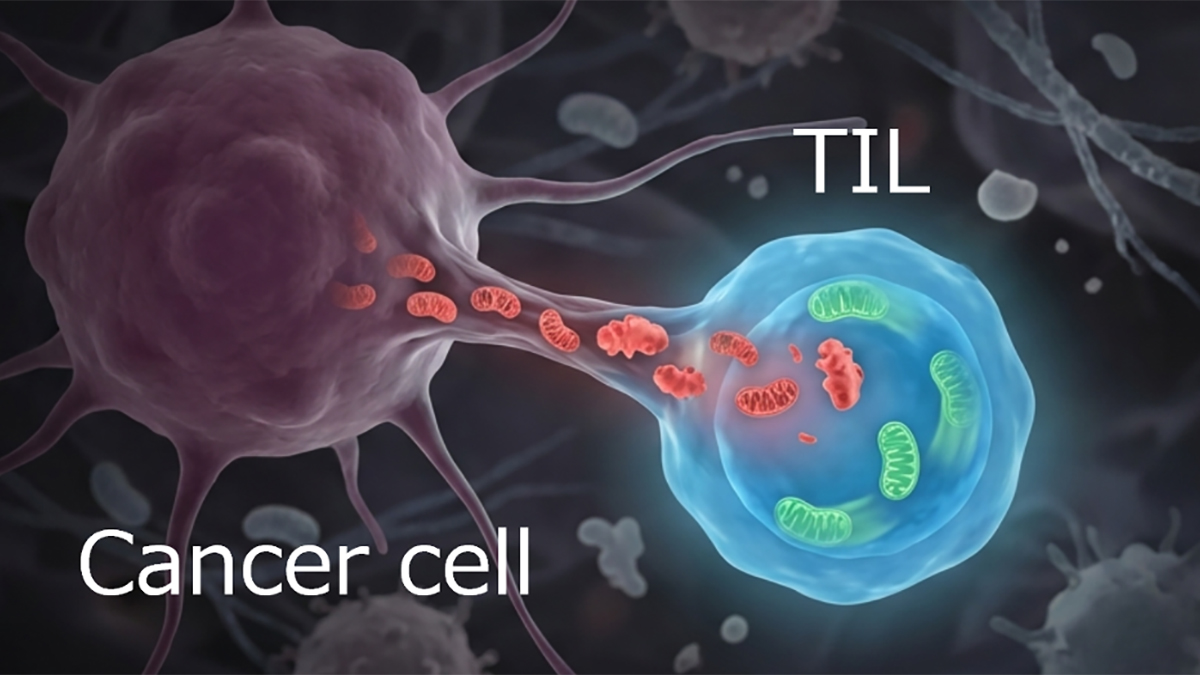
The authors show that effects of space exposure occur in a duration-dependent manner across species and tissues. More specifically, it causes accumulation of reactive oxygen species (ROS) and impairs mitochondrial oxidative phosphorylation (OxPhos), the series of enzymatic reactions that mitochondria use to extract the energy from the food we eat. Moreover, the cellular stress induced by ROS accumulation and OxPhos disruption causes the release of mitochondrial signals that trigger immune system abnormalities in astronauts and animals. Strikingly, the changes to OxPhos and immune activity are accompanied by epigenetic changes that influence mitochondrial gene expression and last for more than 14 weeks after astronauts return to Earth.
The severity of mitochondrial impairment was influenced by the genetic background of the animals exposed to the space environment. Mice with mutations leading to less robust mitochondrial antioxidant defenses against ROS experienced greater damage during space flight, suggesting certain biological pathways can be harnessed to stratify risk profiles and protect astronauts on future missions. To this end, the team tested if kaempferol, an antioxidant compound and stimulator of mitochondrial biogenesis, could reduce the damage from space exposure. Mice treated with kaempferol were protected from liver damage during spaceflight, and human liver organoids exposed to the compound in space lost less mass and retained their function, compared to their untreated counterparts.
This study differs from previous efforts in that it examines changes in mitochondrial biology in response to a range of space-exposure durations across species of animals. It emphasizes the need for and provides evidence of preventative measures and in-flight treatments that can protect astronauts from damage to their mitochondria during longer space missions. These methods and countermeasures will become more important as longer space flights are considered, and they may also shed light on Earth-bound disease mechanisms as well.
Discussion with Drs. Beheshti and Mason
MitoWorld: Space travel seems to affect multiple tissue and organ systems. Could you expand on the mechanisms underlying the effects on mitochondrial function? What work do you think should be done to better understand the conditions that lead to mitochondrial stress?
Beheshti: The two primary stressors in space that drive mitochondrial dysfunction are microgravity and space radiation. In our recent preprint, we highlight how the degree of mitochondrial disruption depends on the radiosensitivity of different tissues, suggesting that some tissues are more vulnerable than others. While both microgravity and radiation are likely to act synergistically, I believe radiation has a more pronounced and compounding impact on mitochondrial health. To better understand these mechanisms, we need studies that systematically compare the effects of microgravity and radiation, both independently and in combination. Additionally, ongoing research, including our own, is evaluating a range of mitochondrial-targeted supplements and therapies as potential countermeasures. I believe there’s strong potential to develop an optimized “mitochondrial cocktail,” a combination therapy tailored to protect against space-induced mitochondrial stress and, ultimately, safeguard astronaut health during long-duration missions.
MitoWorld: Different tissues seem to respond to space exposure in unique ways. Can you speculate on why our organs have different sensitivities to spaceflight? Furthermore, does the stress response to damage in one organ system feed forward to damage otherwise more resilient tissues?
Beheshti: As I mentioned earlier, different organs in the body have varying degrees of radiosensitivity, which helps explain why tissues respond differently to spaceflight. In our recent work, we outline how tissues, such as the spleen, skin, eyes, and immune-related organs, tend to be more radiosensitive, and denser tissues, such as muscle, bone, and brain, are generally more radioresistant. These differences have long been established in the field of radiation biology and translate well to the context of space radiation exposure. However, even the more resistant tissues are not immune. Given prolonged exposure to the space environment, we observed a widespread suppression of mitochondrial OxPhos across all tissues, including long-term effects after returning to Earth.
An important and often overlooked aspect is how damage in one organ system can propagate systemic stress. While we didn’t delve into this in the paper due to limited available data, the concept of a “bystander effect” from radiation biology is highly relevant here. This phenomenon describes how irradiated cells can transmit stress signals to neighboring non-irradiated cells, leading to secondary damage. Similar effects have been observed at the tissue level, suggesting that injury to more radiosensitive organs could exacerbate dysfunction in otherwise more resilient tissues. This kind of cascading, systemic stress response may play a significant role in how the body as a whole reacts to prolonged space exposure, and underscores the need for integrated, multi-organ studies to fully understand and mitigate these complex interactions.
Mason: Each organ system has distinct energetic requirements, and thus, we expect to see some heterogeneity in the response across tissues. Also, each organ ages at different rates, and so, this also is likely a function of mitochondrial function and complex biological interactions across multiple pathways and systems.
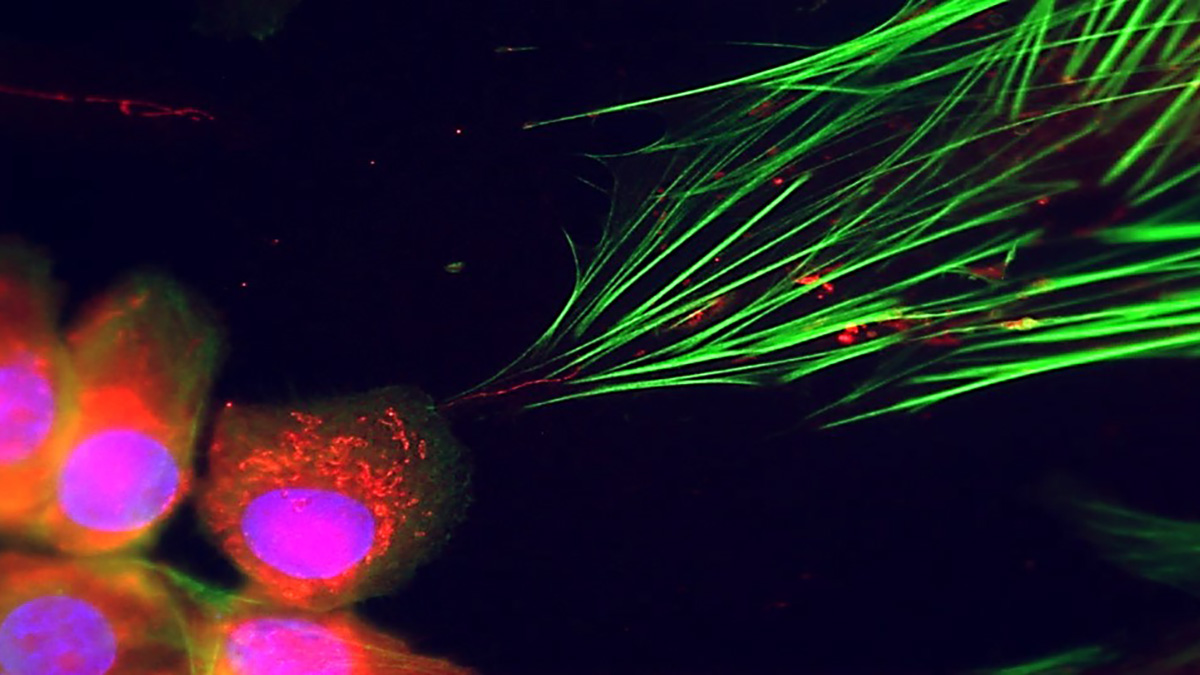
MitoWorld: Does mitochondrial morphology or dynamics change in the low-gravity conditions of spaceflight?
Beheshti: This is an important and still open question. At this time, we don’t have definitive data on how mitochondrial morphology or dynamics change under microgravity conditions, but it’s an area that absolutely warrants deeper investigation. In fact, we are currently conducting imaging experiments to address this very question, and we hope to provide new insights soon. Based on what we know about mitochondrial behavior under various stress conditions on Earth, I strongly suspect that mitochondrial morphology does change in microgravity. Disruptions in mitochondrial fission and fusion dynamics, alterations in cristae structure, and changes in network connectivity are all possible responses to the unique stresses of spaceflight. These changes could have significant downstream effects on energy production, redox balance, and apoptosis, ultimately impacting tissue health and resilience. Understanding these structural and functional adaptations will be key to developing targeted interventions to preserve mitochondrial health in space.
MitoWorld: It’s very interesting that the immune system is affected by mitochondrial stress induced by space flight and that epigenetic changes persist for weeks after astronauts return to Earth. Are returning astronauts more susceptible to infection after long-duration space missions, and does this pose a risk for infections threatening the viability of future space settlements and long-duration travel throughout the solar system?
Beheshti: Our findings suggest that mitochondrial dysfunction, particularly the long-term suppression of OXPHOS, plays a central role in disrupting immune function during and after spaceflight. This mitochondrial stress appears to impair the energy metabolism required for proper immune cell activation and response, leading to broader immune dysregulation. While our study highlights this link mechanistically, it raises the concern that astronauts may indeed be more susceptible to infections after long-duration missions. However, it’s important to note that direct evidence of increased infection rates in returning astronauts is still limited.
What is particularly concerning is that these mitochondrial and immune impairments persist for weeks after return to Earth, and are accompanied by sustained epigenetic changes. This suggests that the immune system does not immediately rebound post-flight, which could pose risks not only upon re-entry but also during extended missions, where access to medical intervention is limited. If such immune vulnerabilities are not properly mitigated, they could threaten the health of crew members and the overall viability of future deep space missions or permanent settlements.
Moving forward, more research is needed to directly measure susceptibility to infection post-flight and to identify reliable biomarkers that flag immune dysfunction early. We must also begin validating countermeasures, including mitochondrial-targeted therapies, that preserve or restore immune resilience in the space environment.
Mason: We don’t see longer risk of infection post-flight, but we and others do see a lot of viral activation in-flight, and changes in biological pathways related to immune function and activation.
MitoWorld: If astronauts, who are selected for being very physically fit and disciplined individuals, suffer ill health effects from long duration space travel, how would the physiological response to long-term spaceflight differ in a cross section of the population?
Beheshti: When it comes to mitochondrial dysfunction, I believe we would see similar core impacts across the general population, but the severity and resilience of the physiological response could vary widely, depending on baseline health, genetic predispositions, and other risk factors. Astronauts are among the most physically fit and medically screened individuals; yet, even they exhibit signs of mitochondrial stress, immune dysregulation, and other health effects during and after long-duration spaceflight. This suggests that members of the general population, who may have pre-existing conditions or less physiological reserve, could be even more vulnerable to the same stressors.
As Dr. Mason pointed out, the Inspiration4 mission, which was the first all-civilian crewed orbital mission, provided a glimpse into how non-career astronauts might respond to spaceflight. While it was a short-duration mission, it offered early indications that space-induced physiological changes are not limited to elite astronauts. If missions extend to months or years, as envisioned for Mars or deep-space travel, we can expect a wider range of biological responses and potentially more severe health challenges in a more diverse population.
This underscores the need for personalized countermeasures and comprehensive health monitoring tools that can accommodate a broader range of individuals. Future missions will likely include people of varied ages, health backgrounds, and genetic profiles. Understanding these differences and proactively developing adaptable therapies, particularly those targeting mitochondrial resilience, will be critical for the success and safety of long-duration human exploration throughout the solar system.
Mason: We saw that the Inspiration4 crew, which was an all-civilian crew, did just fine during a 3-day orbital mission, and so we are cautiously optimistic for future civilian crews. However, as noted above with the murine data and organ risk, the genetic background of the person and other medical factors should all be considered when assessing flight plans.
MitoWorld: This paper showed that an antioxidant and stimulator of mitochondrial biogenesis may have therapeutic benefit for astronauts. Are there any other pathways revealed by your work that you would like to target next to mitigate the damage from spaceflight?
Beheshti: Absolutely. While our study highlighted the therapeutic potential of compounds, such as kaempferol, an antioxidant and activator of mitochondrial biogenesis, our multi-omics analysis revealed additional pathways and molecular targets that warrant investigation as countermeasures. One key area involves the TCA cycle, which we found to be significantly disrupted across multiple tissues post-spaceflight, particularly at later recovery times. This dysfunction alters key metabolites, such as α-ketoglutarate and succinate, that compromise energy metabolism and act as epigenetic regulators, influencing long-term gene expression patterns.
We also observed suppression of mitochondrial protein import machinery (e.g., TOMM20, CHCHD4), MT-ribosome biogenesis, and Fe-S cluster biosynthesis—critical components for maintaining mitochondrial integrity. These are promising intervention points. Another major axis of dysfunction involves sustained activation of the HIF-1α/mTOR pathway, which shifts cellular metabolism from OXPHOS toward glycolysis in a maladaptive response to stress. Targeting this metabolic rewiring could help preserve energy efficiency and reduce cellular senescence.
Additionally, our work showed that mitochondrial damage leads to the release of DAMPs, such as mtDNA and mtdsRNA, which chronically activate innate immune responses (e.g., via cGAS-STING, NLRP3, and RIG-I/MDA5 pathways). This immune dysregulation could be addressed through strategies that reduce mtDAMP release or block downstream inflammatory cascades.
Beyond antioxidants, we’re also exploring:
- SOD2 mimetics (e.g., MnTBAP, EUK8) to reduce oxidative damage,
- MicroRNA-based therapeutics (targeting miR-16-5p, miR-125b-5p, and let-7a-5p),
- PGC1α activators, such as epicatechin or TFEB/NRF1 inducers, and
- regulators of mtDNA replication and repair, including POLG co-factors.
These approaches offer a systems-level path forward. We’re now working to identify synergistic combinations, a kind of “mitochondrial cocktail,” to simultaneously stabilize bioenergetics, dampen inflammation, and promote mitochondrial renewal. These countermeasures are critical for astronaut health during deep space missions and for understanding and treating age-related mitochondrial decline here on Earth.
MitoWorld: You examined an extraordinary number of systems in this paper. What might be the next steps to follow up on this study?
Beheshti: This study was an ambitious effort to map systemic mitochondrial dysfunction across species, but it’s just the beginning. The next logical step is to expand these investigations into additional models that more closely simulate the conditions of deep space, particularly with higher radiation doses and longer exposure durations. These environments will allow us to better assess how prolonged mitochondrial suppression impacts organ function, immune resilience, and aging-like phenotypes.
Equally important is advancing the development and testing of mitochondrial-targeted countermeasures. While our results with kaempferol are promising, a broader, more systematic approach is needed. This includes evaluating combinations of antioxidants, metabolic modulators, gene expression regulators, and mitochondrial biogenesis enhancers across multiple tissues and models. I believe we’re on the cusp of identifying an optimal therapeutic mitochondrial cocktail that could protect against the chronic stressors of spaceflight.
I also want to take this opportunity to invite the broader mitochondrial and space biology communities to join us. Collaboration will be essential to accelerate the development of effective interventions. This is an open call. If you’re working on relevant pathways or therapeutics, let’s connect and build a coordinated strategy to move this field forward together.
Finally, space provides a unique and accelerated model of mitochondrial disease. The dysfunctions we observed in astronauts mirror and, in some cases, intensify those seen in patients with mitochondrial disorders. If we can validate countermeasures that work under the extreme conditions of space, there’s a strong potential to translate those findings back to Earth and develop novel treatments for patients suffering from mitochondrial diseases and related chronic conditions.
Mason: Replication is the cornerstone of good science, and so we want to continue to test these models in future missions, other animal cohorts, and in other cellular contexts.
MitoWorld: Aging induces changes in mtDNA over time and causes changes in the ratio of healthy mtDNA to damaged mtDNA, known as heteroplasmy. Would it be wise in future studies to look at heteroplasmic shifts and if they are permanent or seem to rebound once astronauts return to Earth?
Beheshti: Yes, indeed it will be. We have plans to further explore this.
Mason: Yes, we have seen some evidence of this already from prior missions, and this is an exciting area for future study.
References
1Guarnieri JW, Maghsoudi Z, et al. Guardians of the mitochondria: Space mitochondria 2.0 systemic analysis reveals bioenergetic dysregulation across species. Cell In review.
http://dx.doi.org/10.2139/ssrn.5087025
2Garrett-Bakelman FE, Darshi M, Green SJ, Gur RC, Lin L, Macias BR, McKenna MJ, Meydan C, Mishra T, Nasrini J, Piening BD (2019) The NASA Twins Study: A multidimensional analysis of a year-long human spaceflight. Science 364(6436): eaau8650.